Medication adherence is important for pharmaceutical therapy to be effective in patients with chronic diseases, including diabetes. Medication adherence in diabetics is associated with lower risk for hospitalizations, lower healthcare costs, and lower mortality.
Various publications have reported positive correlations for patient demographics, such as older age, male sex, higher education level, and higher income, with higher adherence to noninsulin antidiabetic medications. On the other hand, patients newly diagnosed with diabetes and taking fewer other medications, retail order prescriptions, and higher member cost sharing were found to be associated with lower medication adherence.
We analyzed one MedInsight® client’s data from 2016 to 2018, with over 3.9 million Medicaid, Medicare, and commercial health plan members, to assess medication adherence in the diabetic population and explore the impact of medication adherence on healthcare utilization. To check medication adherence, we used the proportion of days covered (PDC) concept that measures the number of days filled for chronic disease medication out of the total days under consideration. A PDC or adherence of 80% or more is generally considered the threshold for optimal chronic disease management by various pharmacy quality measure stewards, like the Pharmacy Quality Alliance (PQA).
Medication adherence and patient demographics
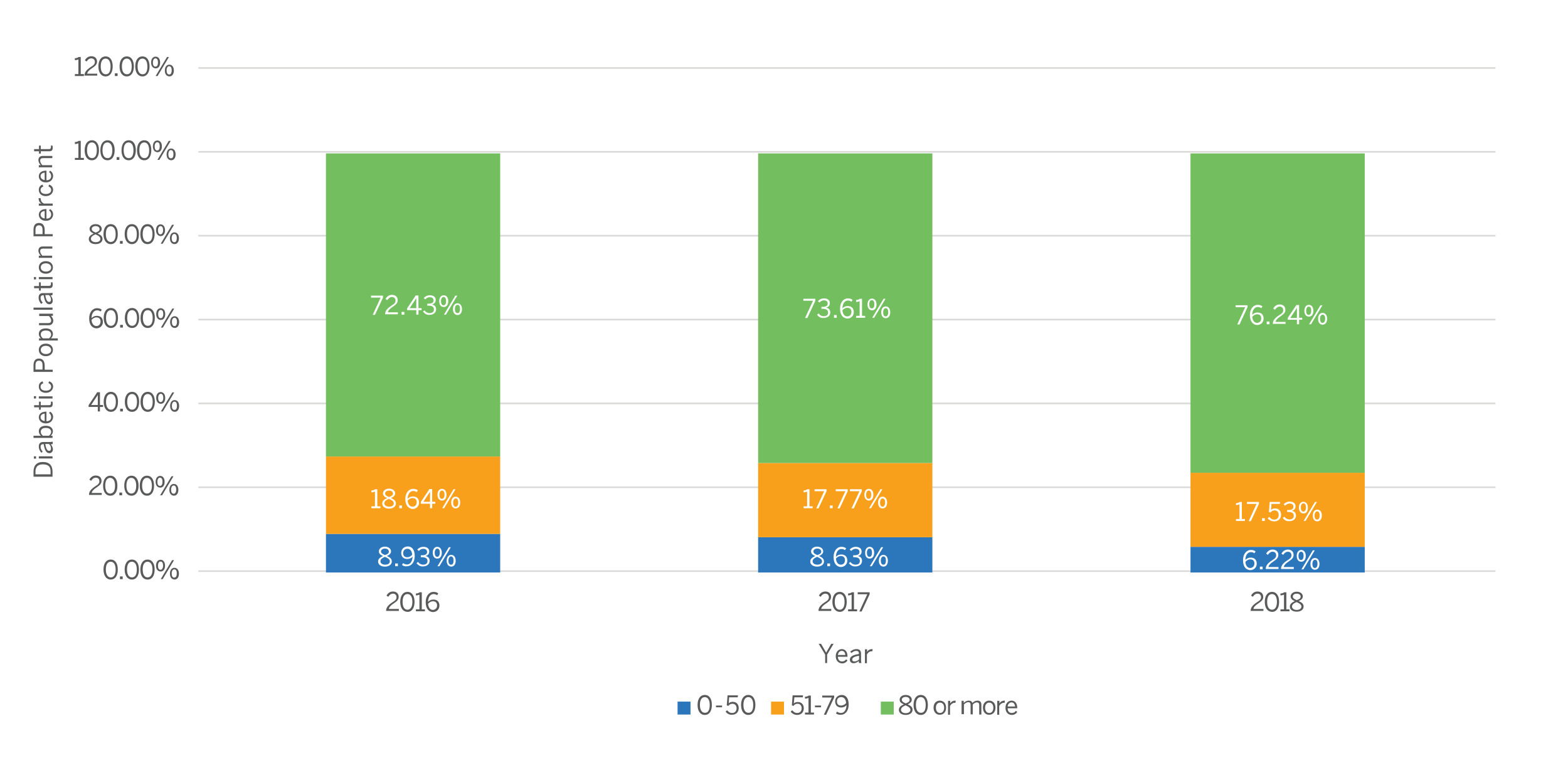
In our analysis from 2016 to 2018, more than 70% of diabetic members had a PDC above 80% each year, with a gradual increase over the three years, as shown in Figure 1.
Figure 1: Diabetic population breakup into PDC categories (2016-2018)
Our observations align with findings from studies highlighting better adherence associated with demographic factors, such as older age, male sex, and higher socioeconomic status:
- A marginally higher proportion of male members (73.9% to 77.5%) had a PDC greater than 80% as compared to females (70.8% to 74.8%) over the analysis period.
- Older diabetic members (above 65 years old) were found to be more active in filling their medication (PDCs of 78.5% to 80.79%) as compared to the younger members (PDCs of 35.5% to 75% for age band 18 and below; 65.9% to 70.7% for age band 19-64 years), across all three years.
- A steep increase in the proportion of members 18 years or younger achieving the recommended PDC was observed between 2016 and 2018 (35.6% in 2016 compared to 75% in 2018).
- A high proportion of diabetic members achieving the recommended PDC were found in Medicare members followed by commercial plan members. This is in line with the impact observed for different age bands. The proportion of Medicaid members achieving 80% PDC stayed below 60% across all three years.
Impact on healthcare utilization
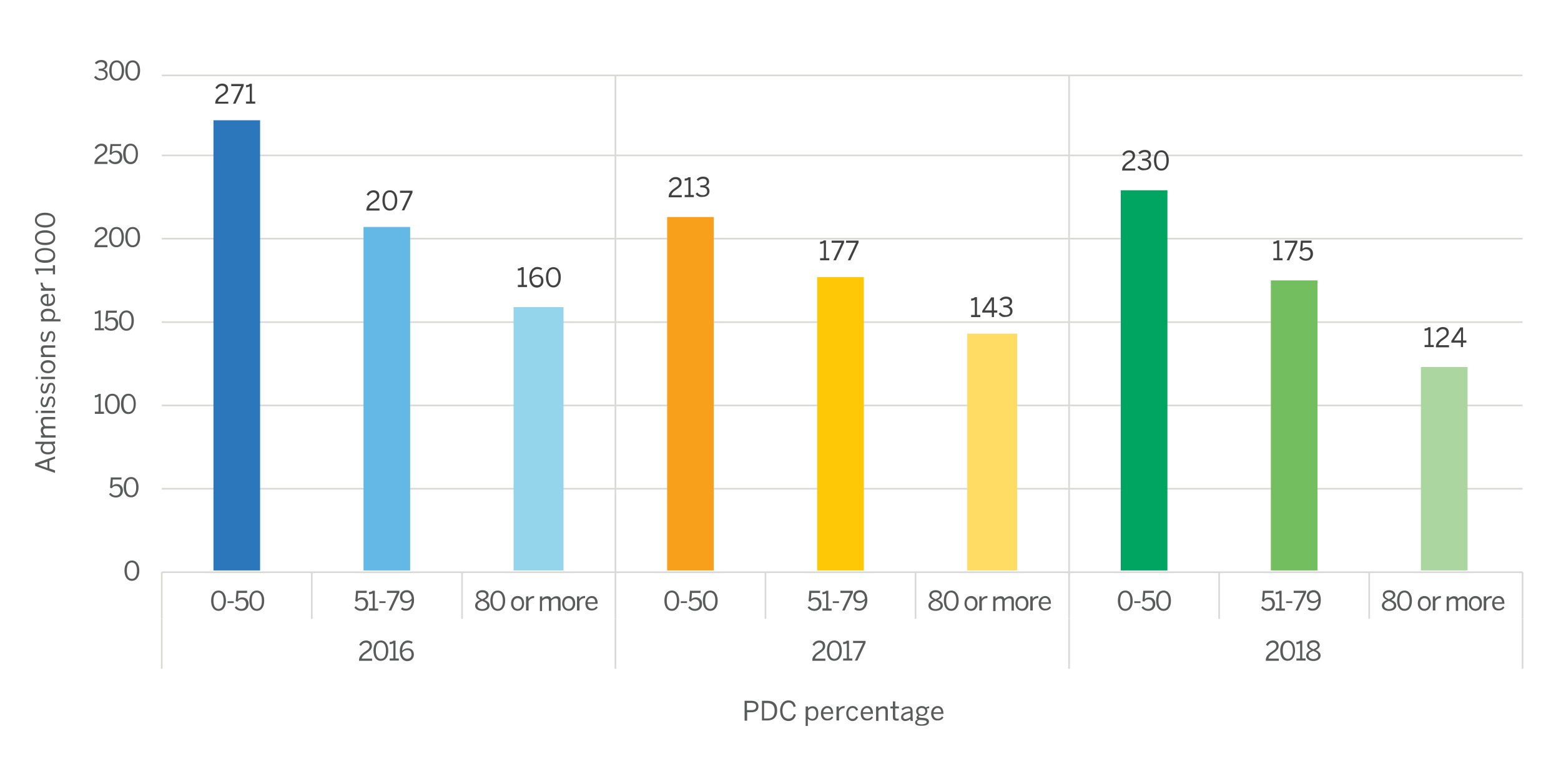
Various studies have demonstrated that adherence to noninsulin antidiabetic medications is associated with more outpatient and fewer inpatient visits, as well as lower total expenditures, as compared to nonadherence. Our analysis reflected similar patterns. Diabetic members with higher PDCs who regularly filled their prescriptions had a lower all-cause hospitalization rate as compared to those who had lower PDCs. Figure 2 shows the comparison.
Figure 2: All-cause hospitalization comparison for different PDC categories (2016-2018)
- In line with the demographic observations, females had 24.4% (2016) to 41.9% (2018) higher inpatient utilization as compared to males.
- Although the older population (65 years and older) had a higher proportion of members with better adherence, they also had 6% to 39% higher inpatient utilization as compared to members 18 to 64 years old. This correlates to the generally higher inpatient utilization in the Medicare population when compared to the commercial population.
Downstream effects
We further analyzed the impact of recommended adherence to diabetes medication on the incidence of short-term and long-term diabetes complications. We found that members adhering to their medication in all three years (2016-2018) were found to have a lower incidence of both short-term complications (STC) and long-term complications (LTC) present in 2018 as compared to members who were not adherent. The difference was significant for STC (0.51% compared to 0.91%) but marginal for LTC (11% compared to 11.8%) and may require a more detailed analysis of longitudinal data for a longer period to get a significant impact of adherence on long-term diabetes complications.
Although the analysis was based on limited administrative data, it illustrated that adherence to medication in diabetes is associated with lower healthcare utilization compared to nonadherence. Despite well-documented benefits of medication adherence in diabetics, adherence to oral antidiabetic agents ranged from 36% to 93% across studies.1 According to one study, the most frequently reported barriers to diabetes medication adherence were found to be forgetting doses (behavioral skills barrier), misinformation on the effectiveness of generic medications versus brand-name medications (information barrier), the false expectation for fast improvement of diabetes right away (information barrier), and feeling burned out with taking diabetes medications.4
MedInsight’s inventory of evidence-based measures (EBMs) has several diabetes adherence-related measures that can be utilized to profile the medication adherence of a diabetic population and design targeted interventions to improve population health.
1 Kirkman, M.S. et al. (2015). Determinants of Adherence to Diabetes Medications: Findings From a Large Pharmacy Claims Database. Retrieved March 16, 2023, from https://care.diabetesjournals.org/content/38/4/604.
2 Pharmacy Quality Alliance. Adherence: PQA Adherence Measures. Retrieved March 16, 2023, from https://www.pqaalliance.org/adherence-measures.
3 Chinthammit, C. et al. (January 2021). Evaluating the relationship between quality measure adherence definitions and economic outcomes in commercial health plans: A retrospective diabetes cohort study. Retrieved March 16, 2023, from https://www.jmcp.org/doi/full/10.18553/jmcp.2021.27.1.064?mobileUi=0&.
4 Nelson, L.A. et al. (August 9, 2018). Assessing barriers to diabetes medication adherence using the Information-Motivation-Behavioral Skills Model. Diabetes Res Clin Pract;142:374-384. Retrieved March 16, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6083841/.